
Gynecomastia
General information
Breast ultrasound examination is essential to establish the diagnosis and differentiate between fatty gynecomastia (pseudogynecomastia, lipomastia) and true (glandular) gynecomastia – the type of treatment depends on the diagnosis.
Types of treatment:
1. Liposuction – fat removal (skin must contract);
2. Surgical removal of the gland only (skin must contract);
3. Additional removal of excess skin as an adjunct to 1 or 2;
4. Various combinations of 1, 2 and 3.
Type of anesthesia
general (anesthesia)
Procedure duration
2 – 4 h
Stay in clinic
1 day
Follow-up examinations
The next day, local condition check, discharge home.
After 1 week (necessary) – local condition check, partial suture removal.
After 2 weeks (necessary) – local condition check, removal of remaining sutures.
One month after suture removal (optional) – local condition, scar, and preliminary assessment of the procedure's outcome.
after 1 year (mandatory) – final assessment of the achieved chest contour and scar.
Medications:
Over-the-counter painkillers
Recovery period after gynecomastia surgery:
Return to intellectual work and driving after 1 week.
Return to light physical exertion and physical work after 1 month.
Gradual increase in loads.
Wearing special compression garment for 1 month non-stop.
Unavoidable consequences of surgery:
General pain and suffering, swelling, bruising, scarring, sensory disturbances in the operated area.
Potential complications:
Hematoma, infection, prolonged wound healing, hypertrophic scar/keloid, skin surface irregularities in the operated area, insufficient correction, overcorrection (indentation), dissatisfaction with the surgical outcome.
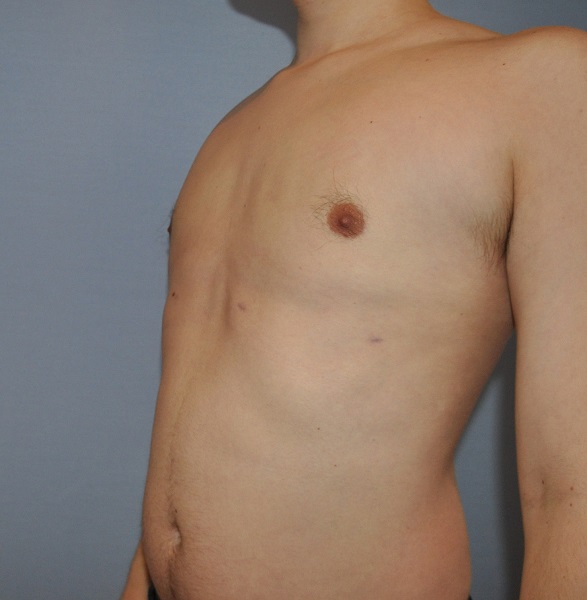
Photo gallery



Detailed information
Gynecomastia, or female breast in a man.
Gynecomastia (literally female breast) is caused by an increase in the volume of the mammary gland. At certain periods of a man's life, gynecomastia is a physiological condition and occurs during periods of hormonal changes: in infancy, during adolescence, and in old age. Gynecomastia often occurs in boys after birth and quickly resolves. However, most cases of gynecomastia occur during puberty. It is believed that an enlarged mammary gland can be found in 65% of boys aged 14-15. By the age of 17, gynecomastia can be found in only 8% of boys. Gynecomastia resolves spontaneously by the end of the second decade of life in almost all young men. The incidence of gynecomastia increases again with age, reaching 30% in older men over 65. Statistics can be misleading as they depend on the criteria for qualifying individuals into the gynecomastia group. It is generally accepted that a mammary gland thickness exceeding 2 cm in a man is a necessary criterion for diagnosing gynecomastia.
It should be emphasized that gynecomastia is, in a sense, normal if it occurs during periods of physiological hormonal changes. Sometimes it can be a result (symptom) of other serious diseases. The cause of gynecomastia can be hormonal disorders resulting from other diseases. Systemic diseases that can cause gynecomastia include: liver diseases in the form of inflammation or cirrhosis, lung cancer, testicular cancer, adrenal tumors, pituitary tumors, colon and prostate cancer, thyroid diseases, testosterone imbalance, congenital syndromes such as Klinefelter syndrome, certain medications and drugs (marijuana, heroin), family predispositions and unknown (idiopathic) causes, as well as diseases generally „weakening” the body (e.g., burns).
There is a generally accepted rule that in cases of gynecomastia during puberty, the patient is observed for 2 years without performing any special diagnostics. During this time, most cases undergo spontaneous regression. If there is no regression, more thorough diagnostics and treatment can be undertaken. In the case of an adult man who suddenly develops bilateral gynecomastia, consultation with an endocrinologist is recommended.
In an adult man (not during puberty) with long-standing (many years) gynecomastia, detailed endocrinological diagnostics are not necessary.
If unilateral gynecomastia suddenly appears in a 30-year-old man, breast cancer should be suspected. One percent of all breast cancers occur in men.
The diagnosis of gynecomastia is established based on a conversation with the patient, breast examination by inspection and palpation, and additional tests. A necessary additional test is breast ultrasonography. Some men presenting to a plastic surgeon due to the presence of „female breasts” have pseudogynecomastia. This is a symmetrical increase in the volume of the male breast caused by fat deposition (and not by glandular enlargement). On palpation in pseudogynecomastia, the breast is soft, and no hard mammary gland is felt. In true gynecomastia, an enlarged mammary gland with increased consistency is palpable. Ultrasonography provides the final confirmation of whether we are dealing with true or pseudogynecomastia. The definitive diagnosis is crucial for choosing the treatment method. In pseudogynecomastia, liposuction can be used to reduce breast prominence, while in true gynecomastia, surgical removal of the gland is indicated.
Gynecomastia is not associated with an increased risk of breast cancer development in men! But if unilateral gynecomastia appears in a man, cancer should always be considered, and this possibility should be ruled out or confirmed!
The type of treatment depends on the diagnosis. In cases of true gynecomastia resulting from systemic diseases or adverse drug reactions, initial treatment should be directed at the underlying disease, of which gynecomastia is only a symptom. In cases of idiopathic gynecomastia (without an identifiable cause) or pseudogynecomastia, the only effective approach is surgical treatment. The type of surgical treatment used depends on the size of the breast prominence, the type of tissue it is composed of (gland or fat), and the amount and laxity of the breast skin.
In cases of pseudogynecomastia, where the breast is not large and the skin is well-toned and elastic, the treatment of choice is liposuction, i.e., the suction removal of excess fat tissue accumulated in the breast area (see liposuction).
In cases of true gynecomastia, where the breast prominence is composed of hard glandular tissue, surgical excision of the gland is necessary. A surgical incision is usually made along the lower semi-circumference of the nipple/areola complex. The scar remains there, but it is barely visible because it is located at the border of the dark skin of the areola and the light skin of the chest.
If the gynecomastia prominence is large with a significant excess of loose skin, it is necessary, in addition to removing the gland, to remove the excess skin. This can often be done through a periareolar incision, although in some cases, breast reduction surgery with additional scars beyond the one around the nipple-areola complex is necessary.
In cases of massive gynecomastia, breast amputation and free nipple-areola complex graft are indicated – as is often done in F/M transsexual patients (see photo gallery: breast amputation in an F/M transsexual patient).
In borderline cases, where the breast prominence is composed of glandular and fatty tissue, liposuction can be performed first, which is effective in most of these cases. Sometimes an additional procedure is necessary to remove the part of the gland that did not respond to liposuction. This can be done during a single operation or spread over stages. The introduction of liposuction in the treatment of gynecomastia has improved the possibilities of gently narrowing the area of excised tissues and allowed for the avoidance of the so-called postoperative „dishing effect”. This means that a clear boundary where the gland was excised is visible on the body surface after the operation.
Preoperative markings (drawing on the patient's body, procedure plan drawn just before the procedure) should be performed with the patient in a standing position with arms along the body. The entire area designated for excision or liposuction should be marked. After markings made with arms along the body, markings should be made again in a standing position with arms raised upwards. Markings in two arm positions allow for a more accurate assessment of the gynecomastia margins.